- Review
- Open access
- Published:
Building a resilient health system for universal health coverage and health security: a systematic review
Global Health Research and Policy volume 9, Article number: 2 (2024)
Abstract
Background
Resilient health system (RHS) is crucial to achieving universal health coverage (UHC) and health security. However, little is known about strategies towards RHS to improve UHC and health security. This systematic review aims to synthesise the literature to understand approaches to build RHS toward UHC and health security.
Methods
A systematic search was conducted including studies published from 01 January 2000 to 31 December 2021. Studies were searched in three databases (PubMed, Embase, and Scopus) using search terms under four domains: resilience, health system, universal health coverage, and health security. We critically appraised articles using Rees and colleagues’ quality appraisal checklist to assess the quality of papers. A systematic narrative synthesis was conducted to analyse and synthesise the data using the World Health Organization’s health systems building block framework.
Results
A total of 57 articles were included in the final review. Context-based redistribution of health workers, task-shifting policy, and results-based health financing policy helped to build RHS. High political commitment, community-based response planning, and multi-sectorial collaboration were critical to realising UHC and health security. On the contrary, lack of access, non-responsive, inequitable healthcare services, poor surveillance, weak leadership, and income inequalities were the constraints to achieving UHC and health security. In addition, the lack of basic healthcare infrastructures, inadequately skilled health workforces, absence of clear government policy, lack of clarity of stakeholder roles, and uneven distribution of health facilities and health workers were the challenges to achieving UHC and health security.
Conclusions
Advanced healthcare infrastructures and adequate number of healthcare workers are essential to achieving UHC and health security. However, they are not alone adequate to protect the health system from potential failure. Context-specific redistribution of health workers, task-shifting, result-based health financing policies, and integrated and multi-sectoral approaches, based on the principles of primary health care, are necessary for building RHS toward UHC and health security.
Background
Resilient health system (RHS) is essential to ensure universal health coverage (UHC) and health security. It is about the health system’s preparedness and response to severe and acute shocks, and how the system can absorb, adapt and transform to cope with such changes [1, 2]. Resilient health system reflects the ability to continue service delivery despite extraordinary shocks to achieving UHC [3]. A study in Nepal showed that adoption of coexistence strategy on the continuation of the international community on strengthening the health sector with the principle of “do-no-harm” and impartiality at the time of conflicts improve the health outcomes [4].
In 2015, the United Nations (UN) General Assembly adopted a new development agenda aiming to transform the world by achieving the Sustainable Development Goals (SDGs) by 2030 [5], based on the lessons from the Millennium Development Goals (MDGs) [6]. The SDGs seek to tackle the “unfinished business” of the MDGs era and recognise that health is a major contributor and beneficiary of sustainable development policies [7]. One of the 17 goals has been devoted specifically to health: “ensure healthy lives and promote well-being for all ages” [6]. All UN Member States have agreed to achieve UHC (target 3.8) by 2030, as part of the SDGs [8]. The 2030 UHC target was intended to reach at least 80% for the UHC service coverage index and 100% for financial protection [9]. Universal health coverage is achieved when everyone has access to essential healthcare services without financial hardship associated with paying for care [10].
Universal health coverage and health security are two sides of the same coin. They are interconnected and complementary goals that require strong health systems and public health infrastructure to ensure that everyone has access to essential health services [11]. Universal health coverage and health security require an integrated and multi-sectorial system strengthening to provide quality and equitable healthcare services across populations [12].
A resilient health system provides the foundation for both [11]. Strengthening the World Health Organisation’s (WHO’s) six health system building blocks, including service delivery, health workforce, health information systems, health financing, leadership and governance, and access to essential medicines and infrastructures are essential to achieve UHC and health security [13]. The 13th WHO programme is structured in three interconnected strategic priorities to ensure SDG-3 including: achieving UHC, addressing health emergencies, and promoting healthier populations [14].
In the World Health Organisation (WHO) European Region, health security emphasises on the analysis of infectious diseases, natural and human-made disasters, conflicts and complex emergencies, and potential future challenges from global changes, particularly climate change [15]. Health security is also considered as the activities required, both proactive and reactive, to minimise the danger and impact of acute public health events that endanger people’s health across geographical regions and international boundaries [16]. The links between health system and health security have started to emerge in several national strategic plans and global initiatives, such as the Global Health Security Agenda (GHSA) and One Health, which aim to better facilitate the implementation of the International Health Regulations (IHR) [17]. The aim of IHR is to prevent, detect, and respond to the international spread of disease in effective and efficient manner [18]. The GHSA also help countries to build their capacity to prevent, detect, and respond to infectious disease threats [19].
Although almost all nations are progressing towards UHC, the advancement in low and low-middle income countries (LLMICs) is slow [20]. This is because the ethos and organisations of many health systems are more suitable for yesterday’s disease burden than tomorrow [21, 22]. Health systems of various nations faced numerous shocks, including public health, social, economic and political crises associated with COVID-19 [23]. The COVID -19 pandemic has made an unprecedented impact on the international community and exposed the vulnerabilities of the present global health architecture [24]. The COVID-19 pandemic is a perfect reminder that countries, individually and collectively, require a strong RHS now more than ever; however, there was no adequate evidence on the strategies toward RHS to improving UHC and health security. Thus, this study can inform the global health community on the lessons of RHS and its applications to UHC in pandemic and beyond. This review generally aimed to address the following research questions: 1) What are the existing evidence on the impact of RHS for UHC and health security? 2) What are the essential elements and characteristics of RHS for UHC and health security as per the WHO building blocks? and 3) What examples exist to demonstrate on how to build RHS core components for UHC and health security?
Methods
Registration and search strategy
This review was conducted and reported following enhancing transparency in reporting the synthesis of qualitative research (ENTERQ). Following ENTERQ guidelines, the systematic review was registered with the international prospective register of systematic reviews (PROSPERO) on 02 January 2022 with registration: CRD42020210471. Studies were searched in three databases (PubMed, Embase and Scopus) using search terms of under four broader domains, including resilience, health system, universal health coverage, and health security. Additional literatures were identified by searching in Google and Google Scholar. The search strategies were built using the four domains of search terms, and “Title/Abstract” by linking “AND” and “OR” Boolean operator terms as appropriate (Additional file 1). We also used the ENTERQ checklist for reporting the articles (Additional file 2).
Inclusion and exclusion criteria
All articles in relation to RHS towards UHC and health security were included in the review. Inclusion criteria were articles written in the English language published from 01 January 2000 to 31 December 2021. Qualitative, quantitative, and mixed methods studies were eligible for inclusion. Exclusion criteria were perspectives, commentary, expert’s opinion, conference papers, debates, conference reports, letters to the editor, and editorials. We presented this paper as a narrative review, following some components of the preferred reporting of systematic review and meta-analysis (PRISMA) guideline for scoping review (Additional file 3).
Selection process
The primary author (AD) imported all retrieved articles into the Endnote library to remove duplicates. After removing the duplicates, three authors (AD, AN and DG) independently screened the articles by title and abstract based on inclusion criteria. The senior authors (RBK and YA) mediated the discrepancies between the three reviewers through discussion. Finally, we retained and reviewed the full texts of all relevant studies for final data synthesis.
Data extraction and framework for synthesis
We used the Rees and colleagues’ appraisal instrument as a guiding tool to appraise the quality of included articles in the review [25]. The quality appraisal instrument is a comprehensive tool designed to assess the quality, rigor of research studies, covers key aspects of research design, data collection, analysis, and reporting. This includes rigour in sampling, rigour in data collection, rigour in data analysis, findings supported by the data, breadth and depth of findings, extent of the study privilege perspectives, reliability or trustworthiness, and usefulness[25]. A template was developed to extract relevant data from each eligible study. After reading the selected studies, key findings were extracted into the template, including information about the first author, year of publication, type of article, study design, and key summary findings. Three independent reviewers (AD, AN and DG) extracted the data. The senior authors (RBK and YA) verified the extracted information. The successes and challenges of RHS for UHC and health security were extracted using health system building blocks.
We analysed the findings using the WHO health system building blocks, including service delivery, health workforce, health information systems, medicines and infrastructures, healthcare financing, and leadership and governance [13]. We analysed the key challenges and successes of RHS for UHC and health security using the WHO health system frameworks. Framework analysis provides a systematic approach to analysing large amounts of textual data using pre-determined framework components. This allows the analyst and those commissioning the research to move between multiple layers of abstraction without losing sight of raw data [26].
Results
Search results
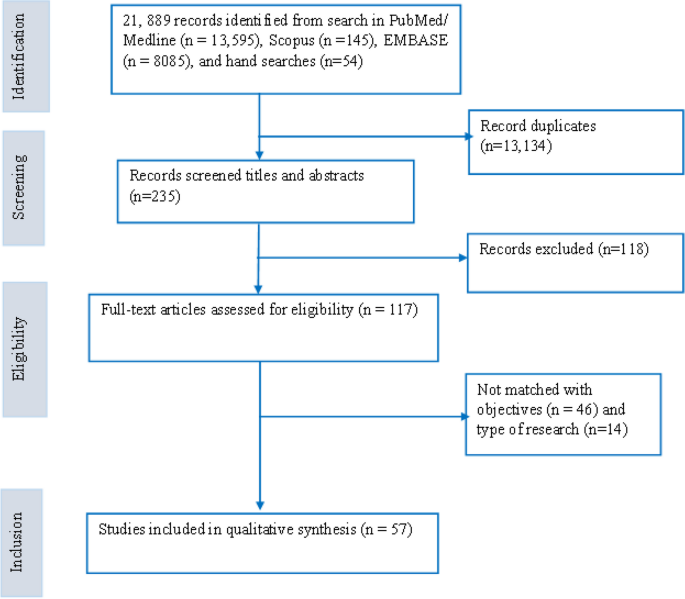
A total of 21,889 records were identified in the initial literature search. After removing 13,134 duplicates, 235 articles were screened by titles and abstracts, and 118 were excluded. Next, 117 studies were reviewed using the full texts, and finally, 57 articles met the inclusion criteria and were analyzed in the systematic review (Fig. 1). Of these, 32 articles were primary studies, and 25 articles investigated the application of RHS on UHC. In addition, nine articles explained RHS's implications on UHC and health security. Of these, approximately one-third (19 articles) were conducted in various African nations, while 19 articles were from Asian countries. The remaining articles were from other parts of the world. The study also reviewed articles on various aspects of health system building blocks, including health service delivery, health workforce, health information systems, health financing, leadership/governance, and medicines and infrastructure. The number of articles reviewed for each aspect were 17, 9, 10, 13, 22, and 10, respectively.
Successes and challenges of RHS
This review used the six-health system building blocks to achieve UHC and health security. These include service delivery, health workforce, health information system, health financing, medicines, diagnostics and infrastructures, and leadership and governance (Table 1).
Service delivery
Of the total reviewed articles, 17 described their healthcare service delivery findings. Good service delivery provides comprehensive and person-centered healthcare services with full accountability [27]. Continuation of healthcare service delivery in the face of extraordinary shocks facilitated UHC progress [3]. Studies reported that health service inputs, access to transportation, communication infrastructures, capacity building, referral systems, intersectoral actions, and electronic healthcare platforms could facilitate service delivery and improve access to health services [13, 28]. Operational integration between health service continuity and emergency response through proactive planning across all income nations reduced health services disruptions during emergencies [29]. Community resources, cohesion, and physical accesses were significant assets to improve service utilisation and quality [30].
An inward migration or mass casualty incidents compromised the quality of services and increased deaths attributed to delays in treatment [30]. In the Ebola crisis, the long-standing lack of access to basic primary health care to isolate and treat infected people fueled the epidemic’s spread resulting in a death toll [31]. Uneven health facilities distribution and lack of well-trained personnel and supplies led to geographical inequities and poor healthcare access [32, 33]. A combination of public health security threats, both new and reemerging infectious diseases, challenged ensuring health security [34]. For example, the health service delivery, mainly the lives of many children, was at risk associated with the lack of treatment for common childhood illnesses in Liberia during the Ebola outbreak [35, 36]. Exclusion from work due to health problems can easily result in economic impoverishment and inequitable healthcare access, which will undoubtedly worsen health status [37]. For instance, socially excluded population groups received health services from a dysfunctional publicly provided health system marked by gaps and often invisible barriers in Guatemala and Peru, which undermines the progress towards UHC [38]. The changes in frequency, intensity, spatial extent, duration, and timing of extreme weather and climate events were also exposed to health threats [39]. For example, extreme weather events caused an increase in disease prevalence, such as malaria and other vector-borne diseases, malnutrition, food insecurity and food-borne diseases [40]. Inadequate primary health care system capacity to provide responsive health services to storm and flood-related health problems was another challenge [41].
Health workforce
In our review, nine articles reported their findings on the successes and challenges of health workforces towards UHC and health security. A well-performing health workforce provides responsive, fair and efficient health services to achieve the best health outcomes [27]. Task-shifting policy, ensuring accountability and ad hoc redistribution of health workers had a knock-on effect on health services delivery and building RHS [42,43,44]. Training on disaster preparedness and management, and rewarding packages, such as incentives and hazard allowance, facilitated healthcare workers willing to participate in disaster management [45]. Monitoring and evaluating frontline health workers levels of preparedness against public health emergency threats periodically by their higher-level hierarchy was crucial for early detection and control of health threats [46].
Lack of skilled and inadequate health workforce distribution was the major obstacle to containing an outbreak, and deaths were attributed to treatment delays [35, 43]. Low perception of risks by tourists/ pilgrims, ineffective training, poor control of risk factors, and shortages of infrastructures were the challenges in combating contagious diseases [47]. Healthcare workers’ practices on effective pandemic management, including corona-virus disease (COVID)-19 were constrained by individual factors, such as education, residence, work station location, hygiene promotion, and social distance management [42]. Patient assessments by non-indigenous health workers during an emergency were also barriers to early identification and management of acute health events [30].
Health information system
In this review, ten articles described the contributions and challenges of health information on RHS to realise UHC and health security. A well-functioning HIS ensures the production, analysis, dissemination and use of reliable information for policy decisions [27]. Building accountability, knowledge culture management, and evidence through regular data quality audit strengthened health management information systems (HMIS) [44]. Integrated disease surveillance, flexible automation and data processing improved clinical care and health system preparedness to tackle health threats [48,49,50]. Strengthening the health system’s capacity was another key measure to rapidly process and communicate test results for pandemic responses [51].
Poor surveillance, late timing of responses and lack of triggers weakened the functionality of plans and exposed to a high burden of diseases [52]. Poor data management, misinformation on the risk and transmission, lack of awareness, resources and insufficient electronic reporting system were responsible for the spread of diseases [51, 53, 54]. For instance, misinformation during the Ebola outbreak affected most communities in putting measures in place to stop the spread of the virus [54]. People approached traditional healers who lacked knowledge on treating certain health shocks in modern medicine was the major problems in early responses [35].
Medical products, diagnostics, and infrastructures
Of the reviewed articles, 10 reported their findings on the successes and constraints of medical products, diagnostics, and infrastructures to realise UHC and health security. Equitable access to essential medical products, vaccines and technologies to assure quality, safety, efficacy and cost-effective healthcare services to users was the attribute of a well-functioning health system [27]. To attain UHC, strengthening local preparedness, planning, manufacturing, and coordinating public–private initiatives and training in LMICs was important [55]. The key factors to facilitate early detection were the provision of rapid, cost-effective, sensitive, and specific diagnostic centers through the inauguration of national centers [53, 56]. Identifying emergency medicines, adaptable mobile health care units and systems for mobilisation of health professionals contributed to successful interventions to curb health emergencies [57].
High patient load, lack of diagnostics, destruction of health facilities and lack of specific funds for medicine procurement may compromise the health system’s hardware (health facilities and supplies) and contained public health threats [3, 30, 32, 57]. For instance, inadequate essential logistics such as blood, oxygen cylinders, ergometrine and sulphadoxine paramita mine in Ghana was the causes for low level of preparedness to control maternal mortality [58]. Shortages of medical supplies, personal protective equipment (PPE), and electricity increased the rate of Ebola infections during the outbreak [35]. Most medicine outlets experienced longer lead times associated with the poor inter-country transportation and limited manufacturing capacity, which were also Namibia's main challenges [55].
Health financing
In this study, 13 articles described their findings on the contributions and limitations of healthcare financing to realise UHC and health security. A good health financing system raised adequate funds for health to ensure people can use needed services and be protected from financial catastrophes [27]. Under a publicly funded health financing system that fits well with values and population preferences improved compliance, sustainability, and equity [59]. An integrated financing mechanism through high income and risk cross-subsidies reduced reliance on OOP payments, maximises risk pools and resource allocation mechanisms facilitated to achieve UHC [60]. Universal health coverage can substantially improve human security through securing finances [61]. Universal health coverage indicators were also positively associated with the gross domestic product (GDP) per capita and the share of health spending channels [62]. Income redistribution improved equity in health care service delivery [63].
Lack of adequate funds and non-affordable medical costs were the main barriers to universal financial protection and poor management of an outbreak [33, 35]. In Burundi, for example, performance-based financing without accompanying access to incentives for the poor was the critical challenge to improve equity in health [64]. Health equity advancement challenges secured dedicated funds to support transformative learning opportunities and build infrastructures [65]. Because of causalities, the health sector requires additional financial support to address the increased demand for health services; however, movement restrictions limit people’s access to participate in gainful activities [30]. Low funds from international donors were erratic and far below the amounts required to meet the health needs at crisis time [66]. People could not trade their commodities because of the fear of attacks exposing service users to lack finances [30]. Falling in financial access to health services has resulted in political demonstrations and violent unrest [67].
Leadership and governance
Our review found that 22 articles reported their findings on health system governance (HSG) to realise UHC and health security. Good HSG ensured strategic policy frameworks combined with effective oversight, coalition, appropriate regulations, system design and accountability [27]. Building strong partnerships, ensuring accountability, coordination, rationalisation, and connection of pandemic planning across sectors and jurisdictions resulted in better preparedness [48, 68]. Clear communication channels, multisectoral, and multilevel controls were essential to translate policy into actions [52, 56]. Vertical and horizontal integration, centralised governance, responsible leadership, and social capital at community level were needed to address health shocks and homogenous implementation of health interventions [54, 69, 70]. Fueling high-performing teams and increasing investment in early warning and detection systems required leadership resilience to enable action at all levels [71, 72].
Working alone the state had proven only partially effective, a situation exacerbated by the natural tendency within the public to ignore as irrelevant to themselves [73]. In addition, lack of clarity of stakeholder roles, poor leadership and absence of clear government policy for the delivery channels and financial coverage led to fragmentation and poor health system response [35, 52, 66]. For instance, weak governance and decision-making processes, such as high bureaucracy, low prevention culture, and lack of coordination between primary, social and hospital care providers, indicated virus’s rapid spread in the French population in the first wave of COVID-19 [74].
Moving away from a one-size fits-to all approach in guiding pandemic response, service delivery, political commitment, fair contribution and distribution of resources are helpful to speed up the path towards UHC [75]. For example, village health volunteers in Thailand, Zanmi Lazante’s Community Health Program in Haiti, Agentes Polivalentes Elementares in Mozambique, Village Health Teams in Uganda, lady health workers in Pakistan, BRAC in Bangladesh, Family Health Program in Brazil, and Health Extension Program in Ethiopia are successful community-based models contributed immensely to achieve health development goals [76]. In addition, community participation and coordination between different stakeholders significantly impact the prevention of encephalitis in Japan [77], and early detection of cases and collection of mortality data in Cambodia [78]. On the contrary, it was difficult for the system to automatically adjust its structure to reduce uncertainty and ascertain complex adaptive behaviour when facing public health emergencies [79].
With an overarching political will, well-integrated and locally grounded health system can be more resilient to external shocks [80]. Political leadership was critical during the crisis, which helped the government to develop a response strategy and effective implementation [81]. For instance, Singapore’s dexterous political environment allowed the government to institute measures to control COVID-19 swiftly [56]. On the other hand, political instability or war in Syria affected healthcare services by destroying physical health care infrastructures [3].
Discussion
In this review, we developed a resilient health system framework that could assist countries in their endeavor toward universal health coverage and health security. The framework involves an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The input components of the framework include health financing, health workforce, and infrastructure, while service delivery is the process component, and UHC and health security are the impact program components. The framework also considers health system performance attributes, such as access, equity, quality, safety, efficiency, sustainability, responsiveness, and financial risk protection. Additionally, the cross-cutting components of the framework are leadership and governance, health information systems (HIS), and contextual factors (e.g., political, environmental/climate, socioeconomic, and community engagement) that can affect the health system at any stage of the program components (Fig. 2).
We also indicated that RHS is critical to achieving UHC because it enables the provision of accessible, quality, and equitable health services, while also protecting people from financial risks associated with illness or injury. Such systems are built on strong primary healthcare services, effective governance and leadership, adequate financing, reliable health information systems, and a well-trained and motivated health workforce [42,43,44]. Resilient health systems are better equipped to deliver high-quality healthcare services to all people, including those who are marginalised or living in poverty. This, in turn, investing in RHS is essential for achieving UHC, promoting health equity, and building more sustainable and equitable societies. On the contrary, lack of healthcare access, skilled health workforces, and uneven distribution of health facilities and health workers [32, 33, 35, 43] were the challenges to achieving health sector goals.
Lack of access, non-responsive and inequitable healthcare services were the challenges to achieve UHC and health security [31,32,33]. Such challenges can be solved by primary health care approach which is an effective strategy to provide accessible, acceptable, equitable and affordable health services to achieve UHC [82, 83]. Community-based and differentiated service delivery models are also important platforms for improving healthcare delivery, access, outcomes, and to meet the specific needs and preferences of different groups of patients [84, 85]. Community-based service delivery model can bring healthcare services closer to where people live and work, and overcome barriers to healthcare access such as transportation, distance, and cost [84]. This service delivery model has also the potential to facilitate a more effective response during healthcare crises by minimising top-down approaches and maximising bottom-up strategies through empowering local communities to take ownership of their health and wellbeing [86]. Additionally, differentiated service delivery model can meet the specific needs and preferences of different groups of patients. For example, providing family planning services within HIV clinics helps women living with HIV to access both services at the same time [85]. Similarly, considering a health system away from a one-size-fits-all approach to healthcare delivery is essential in meeting the needs of diverse patient populations [87].
Lack of skilled and inadequate distribution of health workforces were another major obstacle to contain an outbreak and deaths attributed to delays in treatment [35, 43]. Conducting integrated supportive supervision, maintenance of human resource information systems, and national task shifting policy are important strategies that can help to address critical health workforce gaps and maldistribution [42, 44]. Healthcare workers' pre-service and in-service training opportunities are indeed key to providing quality care. Healthcare workers who receive adequate pre-service and in-service training are better equipped to provide quality care to patients, and also to adapt to new challenges and changing healthcare needs over time [88]. Training in disaster preparedness and offering rewarding packages can also play an essential role in enhancing the willingness of healthcare workers to participate in disaster management [45]. For instance, Kenya's Field Epidemiology and Laboratory Training Program (FELTP) has played a significant role in strengthening the capacity of healthcare workers to detect, document, respond, and report unusual health events [89]. In addition, monitoring frontline health levels is an essential part of preparedness against public health emergencies. This can involve monitoring healthcare facility capacities and the overall preparedness of the healthcare system to respond to an emergency [46].
Poor infrastructure, absence of emergency stockpiles, inadequate logistics, and shortages of medical supplies can be potential obstacles to achieving UHC during health emergencies [30, 35, 57, 58]. A strong public health infrastructure can help to ensure that healthcare resources are distributed equitably, based on need rather than ability to pay. This is particularly important during a pandemic, when resources may be scarce and demand for healthcare services is high [90]. Integrating pharmaceutical supply chain activities with modern technologies and establishing strong relationships between manufacturers, distributors, prescribers, and insurance organizations can help ensure that essential supplies and logistics are available promptly [91]. Efficient procurement and an effective supply chain management system are essential components of a well-functioning healthcare system. They can help ensure that essential medicines, medical supplies, and equipment are available where and when they are needed, which is critical to achieving UHC and providing quality healthcare services to all individuals, regardless of their ability to pay [92].
The main challenges for universal financial protection were inadequate healthcare funds [35]. Context specific health financing mechanisms are essential to provide strong and sustainable health financing and move towards UHC [44, 93]. Additionally, cross-subsidisation from rich to poor and low-risk to high-risk groups provide universal access for the entire population [94]. Similarly, reducing of health systems reliance on OOP payments and maximising risk pools were supportive to achieving UHC [60]. Universal health coverage can play a significant role in improving human security by providing financial protection against the cost of healthcare. In many countries, people face significant financial barriers to accessing healthcare services, and as a result, they may be forced to forgo necessary care or incur significant debt to pay for it. The example of Thailand is a good illustration of the potential benefits of UHC. Thailand implemented a comprehensive UHC program in the early 2000s, which provided coverage for all citizens and legal residents. Over the course of a decade, this program helped to reduce the annual impoverishment rate due to medical costs from 2.71% to 0.49% [61].
Poor leadership and absence of clear government policy led to fragmentation and poor health system response [35, 66]. It is essential to involve a diverse range of stakeholders in pandemic preparedness and response efforts to ensure that a comprehensive and effective response is implemented. Collaborative efforts that include input from various stakeholders are more likely to lead to successful outcomes in mitigating the impact of a pandemic [73, 95]. Good leadership is essential for effective outbreak response because it helps to coordinate and guide the efforts of different stakeholders, including health workers, community leaders, and government officials. A strong leader can help to build trust and confidence among the community, mobilise resources, and ensure that everyone is working together towards a common goal [54]. Health systems governance is essential for creating RHS that can respond to emerging health challenges, such as pandemics, as well as ongoing health concerns. By building strong partnerships and accountability mechanisms, health systems can better address the needs of individuals and communities, and improve overall health outcomes [48]. Cultivating bottom-up and top-down forms of accountability is also important to improve the quality and coverage of health services [96].
This study will provide an insight on RHS framework for achieving UHC and health security with an integrated and multi-sectoral approach that considers the health system building blocks and contextual factors. The limitations of this review include that the study did not quantitatively estimate the extent of resilient health system for UHC and health security. This is because we used articles based on various quantitative, qualitative, and mixed methods. In addition, we used the Rees et al. appraisal instrument as a guiding framework for the eligibility criteria [25]. The Rees specifies some methodological criteria for diverse types of studies but does not have a cut-off point for excluding studies.
This review provides evidence of the successes and challenges of RHS and its impact on achieving UHC globally. The review will also give an insight into the key determinants of RHS to achieve long term health sector goals. It will raise health programmers’ awareness of the importance of RHS and initiate an idea for future discussion and arguments on the subject. The review will also help policymakers and government officials to revise and update their strategic plans and policy directions. This review will also assist policy makers in introducing accountability within public institutions to provide more inclusive and equitable health services without excluding any population groups to achieve UHC. This review will help policymakers to formulate an agreed core set of global and national indicators to improve their health systems performance. This review will also help future researchers as baseline information.
Conclusions
The aspiration for UHC and health security will be realised only through a RHS. Advanced healthcare infrastructures and adequate number of health care workers are essential to build a RHS; however, they are not adequate to protect the health systems from potential failures. The health system’s ideology, traditions in policymaking and management, orientation of service delivery, capacities, motivation, and morale of healthcare workers can affect the nation’s health system. Context-specific redistribution of health workers, task-shifting policy, and result-based health financing policy are helpful in building RHS. It is high time that countries transform their health systems through an integrated and multi-sectoral approach to serve as a road map to realise UHC and health security. We are also recommending for future research studies to focus on building a RHS that can support UHC and ensure health security. Such future studies shall be conducted at the national, regional and sub-regional levels to provide context-specific guidance.
Availability of data and materials
Not applicable.
Abbreviations
- ENTERQ:
-
Enhancing transparency in reporting the synthesis of qualitative research
- GHS:
-
Global health security
- HIS:
-
Health information system
- HRIS:
-
Human resource information system
- HS:
-
Health system
- MeSH:
-
Medical subject headings
- PROSPERO:
-
Prospective register of systematic reviews
- UHC:
-
Universal health coverage
- RHS:
-
Resilient health system
- SDGs:
-
Sustainable development goals
- WHO:
-
World Health Organization
References
Kruk ME, Myers M, Varpilah ST, Dahn BT. What is a resilient health system? Lessons Ebola Lancet. 2015;385(9980):1910–2.
Barasa EW, Cloete K, Gilson L. From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening. Health Policy and Planning. 2017;32(3):iii91–4.
Jamal Z, Alameddine M, Diaconu K, Lough G, Witter S, Ager A, Fouad FM. Health system resilience in the face of crisis: analysing the challenges, strategies and capacities for UNRWA in Syria. Health Policy Plan. 2020;35(1):26–35.
Devkota B, van Teijlingen ER. Understanding effects of armed conflict on health outcomes: the case of Nepal. Confl Heal. 2010;4(1):1–8.
Cf O. Transforming our world: the 2030 Agenda for Sustainable Development. United Nations: New York, NY; 2015.
World Health Organization: Health in 2015: from MDGs, millennium development goals to SDGs, sustainable development goals. 2015.
World Health Organization. Country health information systems: a review of the current situation and trends. Geneva: WHO; 2011.
World Health Organization: Tracking universal health coverage: first global monitoring report: World Health Organization; 2015.
World Health Organization and World Bank. Tracking universal health coverage: 2017 global monitoring report. Geneva: WHO and WBG; 2017.
World Health Organization: Universal health coverage: moving towards better health: action framework for the Western Pacific Region. 2016.
World Health Organization: Building Health Systems Resilience for Universal Health Coverage and Health Security during the COVID-19 Pandemic and beyond: WHO Position Paper.; 2021. In.
World Health Organization: Fostering resilience through integrated health system strengthening: technical meeting report. 2021.
World Health Organization: Monitoring the building blocks of health systems: a handbook of indicators and their measurement strategies: World Health Organization; 2010.
World Health Organization. Thirteenth general programme of work, 2019–2023: promote health, keep the world safe, serve the vulnerable. Geneva: World Health Organization; 2019.
Rockenschaub G, Pukkila J, Profili MC: Towards health security: a discussion paper on recent health crises in the WHO European Region: Bceмиpнaя opгaнизaция здpaвooxpaнeния. Eвpoпeйcкoe peгиoнaльнoe бюpo; 2007.
World Health Organization: The world health report 2007: a safer future: global public health security in the 21st century: World Health Organization; 2007.
Merianos A, Peiris M. International health regulations (2005). The Lancet. 2005;366(9493):1249–51.
World Health Organization: International health regulations (2005): World Health Organization; 2008.
Simo Nikkari KA, Michael Bell, and Karen Sliter,: Global Health Security Agenda pilot assessment of the United Kingdom. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/456984/IndependentReport_GHS_acc.pdf. 2015.
Fullman NLR. Towards a meaningful measure of universal health coverage for the next billion. Lancet Glob Health. 2018;6:e122-123.
Kruk ME, Ling EJ, Bitton A, Cammett M, Cavanaugh K, Chopra M, El-Jardali F, Macauley RJ, Muraguri MK, Konuma S. Building resilient health systems: a proposal for a resilience index. BMJ. 2017;357: j2323.
Hogan DR SG, Hosseinpoor AR, et al.: Monitoring universal health coverage within the sustainable development goals: development and baseline data for an index of essential health services. . The Lancet Global health 2018, 6.
Khetrapal S, Bhatia R. Impact of COVID-19 pandemic on health system & Sustainable Development Goal 3. Indian J Med Res. 2020;151(5):395.
Kishida F: Human security and universal health coverage: Japan's vision for the G7 Hiroshima Summit. The Lancet 2023.
Rees R, Thomas J: Children’s views about obesity, body size, shape and weight: a systematic review [IOE Research Briefing No 49]. 2013.
Ritchie J, Lewis J, McNaughton-Nicholls C, Ormston R. Qualitative research practice: a guide for social science students and researchers. 2nd ed. Thousand Oaks, CA: Sage; 2013.
WHO Everybody’s Business. Strengthening health systems to improve health outcomes: WHO’s framework for action. Geneva: WHO; 2007.
Oppenheim B, Gallivan M, Madhav NK, Brown N, Serhiyenko V, Wolfe ND, Ayscue P: Assessing global preparedness for the next pandemic: development and application of an Epidemic Preparedness Index. BMJ Global Health 2019, 4(1).
Mustafa S, Zhang Y, Zibwowa Z, Seifeldin R, Ako-Egbe L, McDarby G, Kelley E, Saikat S: COVID-19 Preparedness and response plans from 106 countries: a review from a health systems resilience perspective. Health Policy and Planning 2021.
Ager AK, Lembani M, Mohammed A, Ashir GM, Abdulwahab A, de Pinho H, Delobelle P, Zarowsky C. Health service resilience in Yobe state, Nigeria in the context of the Boko Haram insurgency: a systems dynamics analysis using group model building. Confl Heal. 2015;9(1):30.
Heymann DLCL, Takemi K, Fidler DP, Tappero JW, Thomas MJ, et al,: Global health security: the wider lessons from the west African Ebola virus disease epidemic. Lancet 2015.
Omoleke SA, Mohammed I, Saidu Y: Ebola viral disease in West Africa: a threat to global health, economy and political stability. J Public Health Afr 2016, 7(1).
Abiiro GA, Mbera GB, De Allegri M. Gaps in universal health coverage in Malawi: a qualitative study in rural communities. BMC Health Serv Res. 2014;14(1):234.
Rodier G, Greenspan AL, Hughes JM, Heymann DL. Global public health security. Emerg Infect Dis. 2007;13(10):1447.
Shoman H, Karafillakis E, Rawaf S. The link between the West African Ebola outbreak and health systems in Guinea, Liberia and Sierra Leone: a systematic review. Glob Health. 2017;13(1):1.
Siekmans K, Sohani S, Boima T, Koffa F, Basil L, Laaziz S. Community-based health care is an essential component of a resilient health system: evidence from Ebola outbreak in Liberia. BMC Public Health. 2017;17(1):84.
Bejaković P, Škare M, Družeta RP. Social exclusion and health inequalities in the time of COVID-19. Technol Econ Dev Econ. 2021;27(6):1563–81.
Samuel J, Flores W, Frisancho A. Social exclusion and universal health coverage: health care rights and citizen-led accountability in Guatemala and Peru. Int J Equity Health. 2020;19(1):1–9.
Bayntun C, Rockenschaub G, Murray V: Developing a health system approach to disaster management: A qualitative analysis of the core literature to complement the WHO Toolkit for assessing health-system capacity for crisis management. PLoS Curr 2012, 4.
Opoku SK, Hubert F, Adejumo O. Climate change and health preparedness in Africa: analysing trends in six African countries. Int J Environ Res Public Health. 2021;18(9):4672.
Van Minh H, Anh TT, Rocklöv J, Giang KB, Trang LQ, Sahlen K-G, Nilsson M, Weinehall L. Primary healthcare system capacities for responding to storm and flood-related health problems: a case study from a rural district in central Vietnam. Glob Health Action. 2014;7(1):23007.
Seruwagi G, Nakidde C, Otieno F, Kayiwa J, Luswata B, Lugada E, Ochen EA, Muhangi D, Okot B, Ddamulira D. Healthworker preparedness for COVID-19 management and implementation experiences: a mixed methods study in Uganda’s refugee-hosting districts. Confl Heal. 2021;15(1):1–22.
Lehmann U DM, Martineau T, : Staffing remote rural areas in middle- and low-income countries: a literature review of attraction and retention. BMC Health Services Research 2008, 8.
McKenzie A, Abdulwahab A, Sokpo E, Mecaskey JW. Creating the foundation for health system resilience in Northern Nigeria. Health Syst Reform. 2016;2(4):357–66.
Al-Hunaishi W, Hoe VC, Chinna K. Factors associated with healthcare workers willingness to participate in disasters: a cross-sectional study in Sana’a, Yemen. BMJ Open. 2019;9(10): e030547.
Prateepko T, Chongsuvivatwong V. Preparedness against an influenza pandemic of the frontline health facilities in southern Thailand: factor and cluster analyses. Asia Pac J Public Health. 2012;24(1):28–38.
Karampourian A, Ghomian Z, Khorasani-Zavareh D: Exploring challenges of health system preparedness for communicable diseases in Arbaeen mass gathering: a qualitative study. F1000Research 2018, 7.
Ayanore MA, Amuna N, Aviisah M, Awolu A, Kipo-Sunyehzi DD, Mogre V, Ofori-Asenso R, Gmanyami JM, Kugbey N, Gyapong M: Towards resilient health systems in Sub-Saharan Africa: a systematic review of the english language literature on health workforce, surveillance, and health governance issues for health systems strengthening. Ann Glob Health 2019, 85(1).
Dawson G, Gilmour R, Tobin S, Travaglia J: Strengthening public health systems: assessing the attributes of the NSW influenza surveillance system. Public Health Research and Practice 2016.
Lamorde M, Mpimbaza A, Walwema R, Kamya M, Kapisi J, Kajumbula H, Sserwanga A, Namuganga JF, Kusemererwa A, Tasimwa H: A cross-cutting approach to surveillance and laboratory capacity as a platform to improve health security in Uganda. Health Secur 2018, 16(S1):S76-S86.
Fisher D, Hui DS, Gao Z, Lee C, Oh MD, Cao B, Hien TT, Patlovich K, Farrar J. Pandemic response lessons from influenza H1N1 2009 in Asia. Respirology Carlton. 2011;16(6):876–82.
Harrington J, Kroeger A, Runge-Ranzinger S, O'Dempsey T: Detecting and responding to a dengue outbreak: evaluation of existing strategies in country outbreak response planning. J Trop Med 2013, 2013.
Allen HA. Governance and one health: exploring the impact of federalism and bureaucracy on zoonotic disease detection and reporting. Vet Sci. 2015;2(2):69–83.
Alonge O, Sonkarlay S, Gwaikolo W, Fahim C, Cooper J, Peters D. Understanding the role of community resilience in addressing the Ebola virus disease epidemic in Liberia: a qualitative study (community resilience in Liberia). Glob Health Action. 2019;12(1):1662682.
Tirivangani T, Alpo B, Kibuule D, Gaeseb J, Adenuga BA. Impact of COVID-19 pandemic on pharmaceutical systems and supply chain–a phenomenological study. Explorat Res Clin Soc Pharmacy. 2021;2: 100037.
Chua AQ, Tan MMJ, Verma M, Han EKL, Hsu LY, Cook AR, Teo YY, Lee VJ, Legido-Quigley H. Health system resilience in managing the COVID-19 pandemic: lessons from Singapore. BMJ Glob Health. 2020;5(9): e003317.
de Souza THP, Miranda ES. Preparedness of pharmaceutical services in military organizations: learning from an assessment in Brazil. Prehosp Disaster Med. 2020;35(1):24–31.
Amu H, Nyarko SH. Preparedness of health care professionals in preventing maternal mortality at a public health facility in Ghana: a qualitative study. BMC Health Serv Res. 2016;16(1):1–7.
Balabanova D, McKee M. Reforming health care financing in Bulgaria: the population perspective. Soc Sci Med. 2004;58(4):753–65.
McIntyre D, Garshong B, Mtei G, Meheus F, Thiede M, Akazili J, Ally M, Aikins M, Mulligan J-A, Goudge J. Beyond fragmentation and towards universal coverage: insights from Ghana, South Africa and the United Republic of Tanzania. Bull World Health Organ. 2008;86:871–6.
Evans T, Mushtaque A, Chowdhury R: Thailand’s universal coverage scheme successes and challenges—an independent assessment of the first 10 years (2001–2011). Nonthaburi Health Insur Syst Res Off 2012.
Wagstaff A, Neelsen S. A comprehensive assessment of universal health coverage in 111 countries: a retrospective observational study. Lancet Glob Health. 2020;8(1):e39–49.
Starfield B, Birn A-E. Income redistribution is not enough: income inequality, social welfare programs, and achieving equity in health. J Epidemiol Community Health. 2007;61(12):1038–41.
Bonfrer I, Soeters R, Van de Poel E, Basenya O, Longin G, van de Looij F, van Doorslaer E. Introduction of performance-based financing in Burundi was associated with improvements in care and quality. Health Aff. 2014;33(12):2179–87.
Woods-Jaeger B, Daniel-Ulloa J, Kleven L, Bucklin R, Maldonado A, Gilbert PA, Parker EA, Baquero B. Building leadership, capacity, and power to advance health equity and justice through community-engaged research in the midwest. Am J Community Psychol. 2021;67(1–2):195–204.
Ammar W, Kdouh O, Hammoud R, Hamadeh R, Harb H, Ammar Z, Atun R, Christiani D, Zalloua PA: Health system resilience: Lebanon and the Syrian refugee crisis. J Glob Health 2016, 6(2).
Cheng T-M. China’s latest health reforms: a conversation with Chinese Health Minister Chen Zhu. Health Aff. 2008;27(4):1103–10.
Itzwerth R, Moa A, MacIntyre CR. Australia’s influenza pandemic preparedness plans: an analysis. J Public Health Policy. 2018;39(1):111–24.
Prajitha KC, Rahul A, Chintha S, Soumya G, Suresh MM, Nair ANKK, Valamparampil MJ, Reghukumar A, Venkitaraman S, Anish TSN. Strategies and challenges in Kerala’s response to the initial phase of COVID-19 pandemic: a qualitative descriptive study. BMJ Open. 2021;11(7): e051410.
Waitzberg R, Hernández-Quevedo C, Bernal-Delgado E, Estupiñán-Romero F, Angulo-Pueyo E, Theodorou M, Kantaris M, Charalambous C, Gabriel E, Economou C: Early health system responses to the COVID-19 pandemic in Mediterranean countries: A tale of successes and challenges. Health Policy 2021.
Britton CR, Hayman G, Macfarlane C, Alawattegama H, Ballecer J, Stroud N, Wallace A. COVID-19 preparedness and response at a large UK major trauma operating theatres department. J Perioper Pract. 2020;30(7–8):210–20.
Tekola B, Myers L, Lubroth J, Plee L, Calistri P, Pinto J. International health threats and global early warning and response mechanisms. Rev Sci Tech OIE. 2017;36(2):657–70.
Schwartz J, Yen M-Y. Toward a collaborative model of pandemic preparedness and response: Taiwan’s changing approach to pandemics. J Microbiol Immunol Infect. 2017;50(2):125–32.
Or Z, Gandré C, Zaleski ID, Steffen M: France's response to the Covid-19 pandemic: between a rock and a hard place. Health Econ Policy Law 2021:1–13.
Eyawo O, Viens A. Rethinking the central role of equity in the global governance of pandemic response. J Bioethical Inquiry. 2020;17(4):549–53.
Bhutta ZA, Lassi ZS, Pariyo G, Huicho L. Global experience of community health workers for delivery of health related millennium development goals: a systematic review, country case studies, and recommendations for integration into national health systems. Glob Health Workforce Alliance. 2010;1(249):61.
Sahoo KC, Negi S, Dash GC, Sahoo RK, Kshatri JS, Panda S, Pattanaik M, Badaik G, Pati S, Bhattacharya D. Health system preparedness & community participation in Japanese encephalitis/acute encephalitis syndrome (JE/AES) prevention in a tribal district of Odisha, India. Indian J Med Res. 2021;153(3):388.
Oum S, Chandramohan D, Cairncross S. Community-based surveillance: a pilot study from rural Cambodia. Trop Med Int Health. 2005;10(7):689–97.
Wang C, Dong X, Zhang Y, Luo Y. Community resilience governance on public health crisis in China. Int J Environ Res Public Health. 2021;18(4):2123.
Shaikh BT: Strengthening health system building blocks: configuring post-COVID-19 scenario in Pakistan. Primary Health Care Res Dev 2021, 22.
Figueras J, Muscat NA: Health systems resilience during COVID-19: lessons for building back better. European J Public Health 2021:108–108.
Peter T. Exploring taboos: comparing male-and female-perpetrated child sexual abuse. J Interpers Violence. 2009;24(7):1111–28.
Organization WH. Framework on integrated, people-centred health services. Geneva: WHO; 2016.
Lassi ZS, Kumar R, Bhutta ZA. Community-based care to improve maternal, newborn, and child health. Disease Control Priorities. 2016;2:263–84.
Ehrenkranz P, Grimsrud A, Holmes CB, Preko P, Rabkin M. Expanding the vision for differentiated service delivery: a call for more inclusive and truly patient-centered care for people living with HIV. J Acquired Immune Def Syndr. 2021;86(2):147.
Cuthbertson J, Rodriguez-Llanes JM, Robertson A, Archer F. Current and emerging disaster risks perceptions in Oceania: key stakeholders recommendations for disaster management and resilience building. Int J Environ Res Public Health. 2019;16(3):460.
Implementation Guide for Differentiated Service Delivery Models of HIV Services in Uganda. Available at: https://differentiatedservicedelivery.org/Portals/0/adam/Content/FXBRYsohBEGGGiGnnnli3A/File/32.%20Differentiated%20Service%20Delivery%20%20Models%20of%20HIV%20Services%20in%20Uganda%20-%20Implementation%20Guide%207.08.2017-1.pdf
The Global Fund: Focus on Building Resilient and Sustainable Systems for Health. https://www.theglobalfund.org/media/1309/publication_rssh_focuson_en.pdf. 2018.
Roka ZG, Githuku J, Obonyo M, Boru W, Galgalo T, Amwayi S, Kioko J, Njoroge D, Ransom JA. Strengthening health systems in Africa: a case study of the Kenya field epidemiology training program for local frontline health workers. Public Health Rev. 2017;38(1):1–12.
Benjamin GC: Ensuring health equity during the COVID-19 pandemic: the role of public health infrastructure. Revista Panamericana de Salud Pública 2020, 44.
Bastani P, Dehghan Z, Kashfi SM, Dorosti H, Mohammadpour M, Mehralian G, Ravangard R. Strategies to improve pharmaceutical supply chain resilience under politico-economic sanctions: the case of Iran. J Pharmaceut Policy Practice. 2021;14(1):1–14.
The Global Fund: Building Resilient and Sustainable Systems for Health. 2018.
Chu A, Kwon S, Cowley P. Health financing reforms for moving towards universal health coverage in the western pacific region. Health Systems & Reform. 2019;5(1):32–47.
Reich MR, Harris J, Ikegami N, Maeda A, Cashin C, Araujo EC, Takemi K, Evans TG. Moving towards universal health coverage: lessons from 11 country studies. The Lancet. 2016;387(10020):811–6.
Chattu VK, Adisesh A, Yaya S. Canada’s role in strengthening global health security during the COVID-19 pandemic. Global Health Research and Policy. 2020;5(1):1–3.
Fryatt R, Bennett S, Soucat A: Health sector governance: should we be investing more? BMJ Global Health 2017, 2(2).
Acknowledgements
The first author would like to acknowledge other authors for their contribution in searching, extracting, and writing this article. The first author would also extend his gratitude, particularly for the last two senior authors (RBK and YA), for their exceptional dedication in shaping this review.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualisation: AD and YA. Data curation: AD, AN and DG. Formal analysis: AD, AN, DG, RBK and YA. Methodology: AD, AN, DG, RBK and YA. Supervision: RBK and YA. Writing – original draft: AD. Writing – review & editing: AD, AN, DG, RBK and YA.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approvals were not required as the study was a systematic review of articles. The study was registered with PROSPERO number CRD42020210471.
Consent for publication
Not applicable.
Competing interests
All authors declared that they have no competing interest.
Supplementary Information
Additional file 1.
Search strategy.
Additional file 2.
ENTREQ checklist.
Additional file 3.
PRISMA-ScR checklist.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Debie, A., Nigusie, A., Gedle, D. et al. Building a resilient health system for universal health coverage and health security: a systematic review. glob health res policy 9, 2 (2024). https://0-doi-org.brum.beds.ac.uk/10.1186/s41256-023-00340-z
Received:
Accepted:
Published:
DOI: https://0-doi-org.brum.beds.ac.uk/10.1186/s41256-023-00340-z